I have just finished attending the Implementation Science Masterclass 2018 that took place at the Institute of Psychiatry, Psychology & Neuroscience (IoPPN) at King’s College London on the 17th – 18th of July. I thought it would be useful to share some of my notes through some of the tweets I and others shared during the duration of this masterclass.
Before I do that, allow me to share a well used definition of implementation science in healthcare: “Implementation research is the scientific study of methods to promote the systematic uptake of research findings and other evidence-based practices into routine practice, and, hence, to improve the quality and effectiveness of health services and care. This relatively new field includes the study of influences on healthcare professional and organisational behaviour.”
Notes from lectures at the Masterclass
A couple of key slides from the introductory session on Implementation Science by Prof Per Nilsen. #impscim18 pic.twitter.com/leKuQcP3d9
— Dr Salma Patel (@DrSalmaPatel) July 17, 2018
And diff. between clinical research & imp research: imp research focuses on rates of adoption, adherence or fidelity (think of causal change). And efficacy vs effectiveness. #impscim18 pic.twitter.com/hNxPHdEDGI
— Dr Salma Patel (@DrSalmaPatel) July 17, 2018
#impscim18 Slides you’d wish to have developed yourself. Brian Mittman distinguishes btw clinical and implementation research. #impsci pic.twitter.com/tZxvy0NA6p
— Bianca Albers (@Bianca_Albers) July 17, 2018
And finally for today, this looks like a really useful resource from the improvement science team at Kings: https://t.co/Wlwxba6H6M #impscim18
— Dr Salma Patel (@DrSalmaPatel) July 17, 2018
Prof Anne Rogers now talks us through in detail an example of using process evaluation in evaluating a complex intervention #impscim18 #implementationscience pic.twitter.com/vYXPfSjgb5
— Dr Salma Patel (@DrSalmaPatel) July 18, 2018
Prof Curran recommends type 1 hybrid design (test intervention outcomes plus explore implementation-related factors) as a good starting point for researchers new to #ImplementationScience. #impscim18
— Claire Kerins (@claire_kerins) July 18, 2018
Demystifying hybrid effectiveness-implementation studies. We need to ‘translate’ the use of this non-scientific language into other fields of research. Dr Geoff Curran’s wonderful slide #impscim18 pic.twitter.com/uqqTrYlgNE
— Claire vd Westhuizen (@InjuryDocClaire) July 18, 2018
The very final session is on funding opportunities for imp science from @NCICareDelivRes More info here: https://t.co/oUOrDJ5fsb #impscim18 #implementationscience
— Dr Salma Patel (@DrSalmaPatel) July 18, 2018
Check out King’s resources about improvement and implementation #impscim18 @KingsCollegeLon https://t.co/ydi2tSHQSF pic.twitter.com/Az2UB76yWi
— Olivia Biermann (@olibiermann) July 17, 2018
Notes from workshops at the Masterclass
Workshop 1: Learning healthcare systems – Prof Brian Mittman
Key notes from the session: We can and should be taking advantage of data that we routinely collect when delivering care, and learning from it to generate new knowledge. Sounds like a simple concept, but there are barriers to implement it, and the standards we have in our integrated delivery system are not always what the researchers need. High performing healthcare systems have embedded research, have mechanisms embedded to improve quality and benchmarking information. Another element is innovation, you need internal capacity to innovate, and decide whether they are successful or not, you also need capacity to scan the environment to look for external innovations, you need capacity to do PPI, train staff etc.
Workshop 2: Engaging stakeholders – from patients and the public to policy makers and practitioners – Prof Annette Boaz
Thinking about stakeholder engagement – useful tool. Thanks, @AnnetteBoaz #impscim18 pic.twitter.com/ghNDcHVcsi
— Claire vd Westhuizen (@InjuryDocClaire) July 18, 2018
#impscim18 @AnnetteBoaz on ways of working with stakeholders pic.twitter.com/bb9jS84QY1
— Better Conversations (@BCAphasia) July 18, 2018
Workshop 3: Getting implementation research published – Profs Greg Aarons and Nick Sevdalis
@NickSevdalis reminds researchers (especially early career) about the long journey to publication. Realistic expectations are key here, definitely something I have been learning over the course of my PhD #phdchat #impscim18 pic.twitter.com/ltMENsiQwa
— Beatriz Goulao (@beagoulao) July 18, 2018
IMRaD your paper to ensure a coherent & useful structure @NickSevdalis #impscim18 Can I use it as a verb?! 😉 pic.twitter.com/Gx9cD3SHYk
— Beatriz Goulao (@beagoulao) July 18, 2018
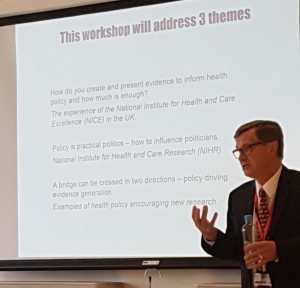
Workshop 4: Bridging the gap between research and policy – Prof Peter Littlejohns
This session was led by Prof Littlejohns who was a founding director of NICE. He believes NICE was developed as a policy maker, and not just guidance. These three themes were covered in this session:
 Prof Littlejohns also recommended reading these papers:
Prof Littlejohns also recommended reading these papers:
- Conceptualizing and Combining Evidence for Health-System Guidance, May 31, 2005 by Jonathan Lomas, Anthony Culyer, Chris McCutcheon, Laura McAuley, Susan Law: https://www.cfhi-fcass.ca/migrated/pdf/insightAction/evidence_e.pdf
- What makes an academic paper useful for health policy? By Christopher J. M. Whitty https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-015-0544-8

Comments